You know how sometimes after a bad day, a glass of wine can help you temporarily escape your troubles? Well, while alcohol might provide fleeting relief, relying on it too much can actually make depression worse in the long run. In this article, we’ll explore the following:
- The complicated relationship between alcohol and depression.
- The science behind why they’re such a dangerous combination for some people, as well as the most effective substance abuse treatments for those struggling with alcohol abuse and depression.
- Healthy coping strategies to deal with stress without hitting the bottle.
Even if you don’t have clinical depression, this article will give you insight into how alcohol abuse affects your mood and motivation. Let’s dive in and shed some light on the depressant qualities of America’s favorite drug.
Alcohol Is a Depressant That Can Worsen Depression
It Directly Impacts Brain Chemistry
You might think alcohol gives you a buzz, but it’s actually a depressant. That means it slows down activity in your brain and central nervous system. So while drinking may make you feel relaxed at first, it disrupts the balance of neurotransmitters like serotonin and dopamine that regulate mood.
This throws your brain chemistry out of whack. Over time, heavy alcohol use can lead to deficiencies in these “feel-good” chemicals, increasing feelings of sadness, anxiety and hopelessness. Not a great combo with depression!
Alcohol Worsens Symptoms
Drinking heavily while depressed is like adding fuel to the fire. Alcohol can amplify common symptoms like fatigue, irritability, sleep issues and difficulty concentrating. It can also increase impulsive behavior, making you more likely to act recklessly or have suicidal thoughts when feeling down.
The hangover and withdrawal effects just compound the problem. As alcohol leaves your system, you may feel even more depressed, anxious and lethargic. This vicious cycle makes it harder to manage your mood and function normally.
Alcohol Reduces Medication Effectiveness
Many people take antidepressants or other psychiatric medications to treat depression. But alcohol can render these drugs less effective or cause dangerous interactions. It changes how your body metabolizes the medicine, reducing its therapeutic benefits.
Some antidepressants can also amplify the sedating effects of alcohol, putting you at risk of overdose. Not exactly a recipe for healing from depression! Managing your condition becomes much more difficult when mixing alcohol with medication.
The Connection Between Alcohol and Depression
A Dangerous Cycle
You may have heard that alcohol is a depressant. But the connection between drinking and depression goes much deeper than that. Frequent or excessive alcohol use can actually trigger or worsen symptoms of depression. And people struggling with depression are more likely to turn to alcohol as an escape or coping mechanism, creating a vicious cycle.
Alcohol’s Effects on the Brain
Alcohol is a central nervous system depressant that slows brain activity. In the short term, it can cause mood changes like increased sadness or anxiety. Over time, heavy drinking actually alters brain chemistry and neural pathways linked to depression. It depletes serotonin and other neurotransmitters that regulate mood.
A Dual Diagnosis
When someone suffers from both an alcohol use disorder and depression, it’s known as a dual diagnosis or co-occurring disorders. These conditions feed off each other, making both harder to treat. Depression fuels alcohol abuse as a form of self-medication. And alcohol abuse exacerbates depressive symptoms. Breaking this cycle requires comprehensive, integrated treatment for both issues simultaneously.
Get Help Today
If you or a loved one is caught in the tangled web of alcohol addiction and depression, don’t wait to seek professional help. Specialized dual diagnosis programs provide evidence-based therapies, group therapy, and other resources. With the right treatment plan, it’s possible to heal and achieve lasting recovery from both disorders.
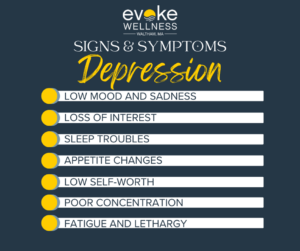
Signs and Symptoms of Depression
Low Mood and Sadness
You feel down, empty or sad most of the time. Simple pleasures in life don’t bring you joy anymore. This low mood lingers for weeks or months on end.
Loss of Interest
Things you once enjoyed like hobbies, work or being with loved ones no longer interest you. It’s hard to motivate yourself and you’ve lost your zest for life.
Sleep Troubles
You either sleep too much or have insomnia – tossing and turning through the night. Your sleep patterns are completely disrupted and leave you fatigued during the day.
Appetite Changes
Your appetite dwindles and you lose weight without trying. Or the opposite – you overeat and rapidly gain weight as food becomes an unhealthy coping mechanism.
Low Self-Worth
You feel worthless, guilty and overly self-critical. These negative thoughts about yourself make it hard to function normally day-to-day.
Poor Concentration
It’s difficult to focus, make decisions or remember things. Simple tasks seem mentally draining. You may struggle at work or school.
Fatigue and Lethargy
You have little to no energy and feel physically drained most days. Even small tasks exhaust you and sap your motivation to do anything.
Dangers of Mixing Alcohol and Depression
An Unhealthy Combination
Trying to cope with depression by drinking alcohol is a risky move that can make your symptoms worse. Alcohol is a central nervous system depressant that slows brain activity – the opposite of what you need when you’re already feeling down. It may provide temporary relief, but when the alcohol wears off, your depressive symptoms return with a vengeance.
A Vicious Cycle
Drinking heavily when depressed creates a vicious cycle that’s hard to break. You drink to escape your negative feelings, but the alcohol ends up intensifying those emotions. As you feel even worse, you’re tempted to drink more, falling into a self-destructive pattern.
Dangerous Interactions
Many antidepressant medications shouldn’t be mixed with alcohol, as it can cause dangerous side effects or make the drugs less effective. Check with your doctor about safe consumption levels. The combination is also linked to impaired memory, slowed thinking, and increased suicide risk among depressed individuals.
Getting Treatment for Alcohol Addiction and Depression
Seek Professional Help
If you’re struggling with alcohol addiction and depression, it’s crucial to seek help from a mental health professional. These are serious issues that require expert guidance and support. Don’t try to tackle them alone.
Therapy Options
Cognitive behavioral therapy (CBT) and dialectical behavior therapy (DBT) are effective for treating both alcohol addiction and depression. A therapist can help you develop coping strategies, identify negative thought patterns, and make positive changes.
Support Groups
In addition to therapy, joining a support group can provide a sense of community and accountability. Alcoholics Anonymous (AA) and depression support groups allow you to connect with others facing similar challenges.
Medication Management
In some cases, your doctor may prescribe medication to help manage depression symptoms or reduce cravings for alcohol. However, it’s essential to follow the treatment plan carefully and never mix medications with alcohol.
Lifestyle Changes
Making lifestyle changes can also play a vital role in recovery. Exercise, a healthy diet, good sleep habits, and stress management techniques can all contribute to improved mental health and reduced alcohol dependence.
Be Patient and Persistent
Recovery is a journey, not a destination. It takes time, effort, and persistence to overcome alcohol addiction and depression. Be kind to yourself, celebrate small victories, and don’t get discouraged by setbacks. With the right support system and commitment, you can regain control of your life.
Frequently Asked Questions About Alcohol, Depression and Treatment
Is alcohol itself a depressant?
Yes, alcohol is classified as a depressant drug because it slows down brain activity and bodily functions. It can amplify feelings of depression and sadness, even in people without clinical depression. When you drink alcohol, it disrupts the delicate balance of neurotransmitters and receptors in your brain that regulate mood.
Can drinking lead to depression?
Absolutely. Heavy, long-term alcohol use can directly cause clinical depression by altering brain chemistry. Alcohol abuse can also trigger or worsen existing depression. Using alcohol to try to “self-medicate” depression is extremely risky and counterproductive.
Will quitting alcohol cure my depression?
Quitting alcohol alone may not immediately relieve depression symptoms, but it’s a crucial first step. Continued alcohol abuse perpetuates the vicious cycle of depression. Getting sober allows your brain to start healing itself and respond better to therapy, medication, or other depression treatments.
What’s the link between alcoholism and suicide?
People with alcohol use disorders have much higher rates of suicidal ideation and suicide attempts. Alcohol is a major risk factor for suicide, as it can intensify hopelessness and impulsivity. If you or a loved one are having suicidal thoughts, seek immediate professional help.
Do I need to go to rehab?
Alcohol rehab programs provide a safe, supportive environment to get sober and get any co-occurring mental health issues like depression properly diagnosed and treated. Outpatient rehab is an option if your alcohol use and depression are less severe. Ask your doctor about the level of care that’s best for you.
Start Your Journey with Evoke Wellness at Waltham
If you or a loved one is considering substance abuse treatment, Evoke Wellness at Waltham invites you to contact us. Our compassionate team is ready to answer your questions, discuss your needs, and help you take the first steps toward recovery. At Evoke Wellness, you will find more than just a treatment program – you’ll discover a community dedicated to your wellness and success. Together, let’s embrace the journey to recovery and the promise of a new beginning. Call us at (833) 287-7223 today or reach out online.